I Almost Died From Endocarditis- and I Had Never Heard of It
One of the lesser-known complications of IV drug use, even among intravenous users is a disease called endocarditis. In 2016, I contracted bacterial endocarditis and it came within hours of killing me. In this post, I’m going to tell you what endocarditis is, what signs and symptoms to look for and how lower the chances of getting it.
Let’s face it, even staring down the barrel of a 29 gauge syringe knowing it’s loaded with a lethal dose- an addict in active addiction is still going to push the plunger if he or she is in withdrawal. Knowing this from personal experience, I feel that it’s important to at least lower the chances someone gets bacterial endocarditis if they are not ready to put the needle down.
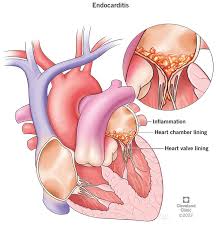
What is Bacterial Endocarditis and How do You Get It?
I had been using needles to inject heroin, cocaine and pharmaceutical drugs like Oxycodone and Morphine for over a decade before I learned what bacterial endocarditis was. My learning experience came at the price of a four month stay in the University of Vermont Medical Center where they replaced my Mitral Valve and pumped me full of IV antibiotics through a PICC line.
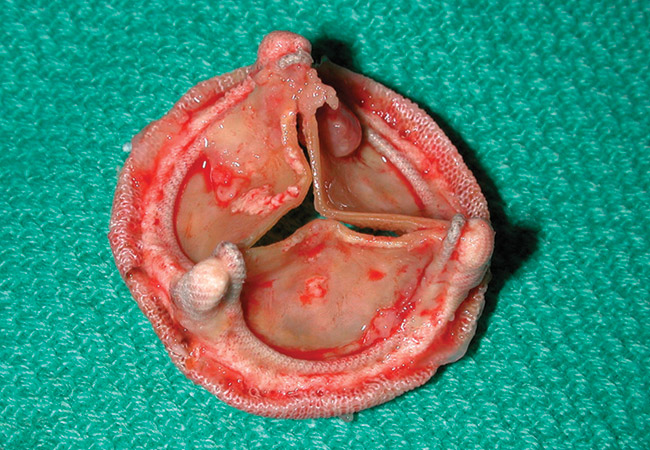
Bacterial endocarditis occurs when bacteria invades the bloodstream and attaches itself to one of the valves in a persons heart, whether it be the Mitral, Aortic, Bicuspid or Tricuspid and grows into what’s called a vegetation. In my case it was the size of a softball and it chose the mitral valve to call home.
What Happens When You Get Endocarditis?
Endocarditis is a very serious illness and left untreated, it will kill you and very quickly if the strain of bacteria is aggressive enough. When I got endocarditis, it was due to a staphylococcus aureus bacterial infection that travelled from my blood to my heart. The staph infection in my blood wasted little time growing in my blood and latching on to my heart valve causing what is known as “regurgitation”– a condition in which a persons blood actually flows back through the valve into the heart instead of flowing properly to the rest of your body.
What Were the First Symptoms of Endocarditis?
I can remember the first symptom of bacterial endocarditis that I experienced just like it happened yesterday. At the time of course, I just shook it off as a symptom of my obviously unhealthy lifestyle or even a common cold. In hindsight, I now know that the cold shivering I experienced at work was just the start of what would be a rapidly progressing illness. Here are the first signs and symptoms I experienced when I got endocarditis.
1). Shivering, Fever-ish feeling
Standing at the cash register of the store I was working at, I broke out in a quick but intense bout of shivering. It was the same type of shiver that you get when the flu onsets and your body temperature rises due to fever. If you have ever had “cotton fever”, the shivering associated with early-onset of bacterial endocarditis is very similar.
2). Intense Fatigue
A couple days (in which I felt decent, all things considered) after I developed those fever-ish symptoms, I started to feel extremely fatigued. I was using an obscene amount of stimulants the day leading up to this night that I vividly remember but even without the use of any opiates, I could not keep my eyes open. It was this night that the symptoms of my infective endocarditis (IE) intensified to the point that over the next couple days it almost killed me.
3). Osler Nodes and Janeway Lesions
One thing that I did not notice until after I was carried into the hospital by my father with a fever over 105º was what are called Osler nodes and Janeway lesions. What causes these Osler nodes is when pieces of the vegetation growing in a person with infective endocarditis’s heart start to spray off and make their way to the hands and feet or what specialists call extremities.
What do Osler Nodes and Janeway Lesions look like?
In terms of appearance, Osler Nodes and Janeway Lesions look very similar to a blood blister but they appear in the absence of any type of trauma. The difference between a Janeway lesion and an Osler node is the former is non-tender where an Osler node tends to be tender to the touch.

The problem with Osler Nodes as a way to diagnose endocarditis is they usually develop in later stages of the disease which makes identifying them a hard way to diagnose endocarditis before it becomes life-threatening. The two skin conditions almost always manifest in acute endocarditis. This is why I did not notice these two symptoms of my own infective endocarditis until after I was already hospitalized and awaiting a mitral valve replacement.
How is Infective Endocarditis Treated or Cured?
There are two types of infective endocarditis– acute and subacute. Both levels of disease are treated and cured in different ways depending on severity and how far the bacteria causing the infection have spread and multiplied. One course of treatment involves an intense regimen of intravenous antibiotics and the other requires open-heart surgery to replace the infected heart valve along with the antibiotic regimen to prevent recurrence.
1). IV Antibiotics to Treat IE
If the recommended course to treat your infective endocarditis involves IV antibiotics only, it’s likely you will be confined to a hospital for 12-16 weeks with a PICC line installed to deliver the antibiotics straight into an artery.
Due to the harsh antibiotics used to treat endocarditis such as Vancomycin and Gentamicin, most health care providers will install a PICC line to save the patients veins. Because of the high potential that an IV drug user will abuse access to the PICC, it will almost always be required the patient be hospitalized throughout the entire course of antibiotics.
2). Open-Heart Surgery for Valve Replacement
The second most common treatment for infective endocarditis, especially acute endocarditis is a valve replacement requiring open-heart surgery or at the very least a laparoscopic procedure. In this scenario, you will also have to endure the intense regimen of IV antibiotics to prevent recurrence of the endocarditis.
In most cases, the surgeon assigned to a patient with IE due to intravenous drug-use will opt for what’s called a “pig-skin or cow valve”, essentially a prosthetic valve made out of porcine or cow tissue. For that reason, a pig can also be called a tissue valve.
If you are lucky and the surgeon believes that you can make significant changes in your lifestyle, he or she may opt to use a mechanical heart valve which is meant to last a life-time if cared for properly. I was given this chance and as much as I hate to admit it- the surgeon made the wrong choice. I have relapsed repeatedly since being given a mechanical heart valve and by the grace of something much bigger than me, I am still here.
I am the outlier though. People can and do die every day due to infective endocarditis and most of them never even knew that it existed. That’s why it’s my goal to inform people with this post.
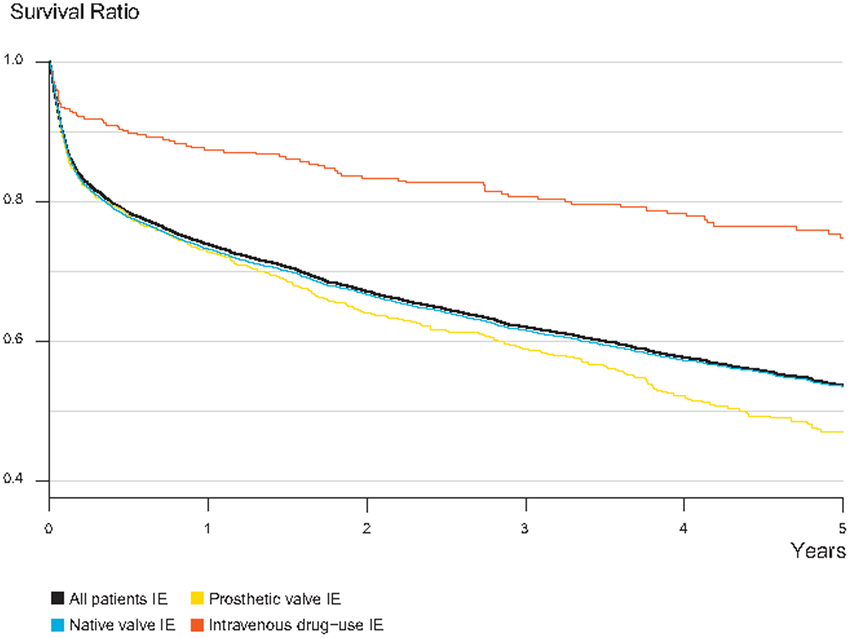
What is the Survival Rate of Infective Endocarditis?
Survival rates for patients after infective endocarditis vary according to who you ask, but one thing is concrete. Continued IV drug use after contracting IE- even after having heart surgery to remove the infection- leads to extremely low survival rates. Some estimates put the ten-year survival rate in IV drug-users diagnosed with endocarditis as low as 44%.
Three year mortality rates post-surgery are often higher than 30% and the risk obviously correlated to a change in lifestyle habits and whether or not the person continues to use drugs intravenously after the initial diagnosis and subsequent treatment.
How to Lower the Chances of Getting Endocarditis
Im actually conflicted about even writing about ways to lower the chances of or prevent endocarditis because I would rather scare an IV drug user into putting the needle down, but I’m also realistic enough to know that most won’t. I’m also a proponent of harm-reduction for IV users because that every life, no matter how screwed up deserves a chance to be saved like I was on the several occasions that I overdosed on Fentanyl and when I almost died of complications due to endocarditis.
So instead of preaching in this post, I’m going to instead spread some ideas for proper hygiene that might lower the odds an IV drug user gets endocarditis. Not one single or combination of measures can fully prevent endocarditis in intravenous drug users, so don’t ever be fooled into thinking you are safe until you stop poking holes in your skin. Here are some things you can do to help lower the chances that you will contract a deadly heart valve infection.
1). ALWAYS use a new syringe.
It should be common practice to use new syringes every time a user injects but unfortunately it is not and the desperate nature of addiction makes it likely that at some point you are going to use a syringe that is not sterile.
In todays harm-reduction society there are many ways to get clean syringes, but rural areas and a lack of transportation makes it likely that many addicts will be re-using syringes sometimes to the point that they have to be forced through the skin. I’ve done it, I’m sure you have also but it should ALWAYS be avoided in favor of using a brand new sterile “rig” when possible.
If a new, sterile syringe is not an option and you are going to use an old one- after all options have been exhausted- at least clean the old needle. It’s important to sterilize the inside of the chamber, but it’s pertinent that you also sterilize the needle itself to prevent bacteria from entering your blood stream.
2). Prep and Clean the Injection Site
After you have sourced a new syringe to inject with, the next thing that needs to be done to lessen the likelihood of introducing bacteria is to clean the injection site with an alcohol prep pad like the ones used by phlebotomists. These are extremely cheap and if you can’t find them, a bottle of rubbing alcohol will serve the same purpose as long as you are generous and do not touch the site afterward.
3). Always Use Sterile Equipment

Its common practice among IV users to mix their shot in a spoon or the bottom of an aluminum can. Doing this is a no-no and has a much larger potential to introduce fungus or bacteria that can cause endocarditis. It’s always safest to make sure that everything including the water you mix a shot with are 100% sterile.
In larger cities and some rural areas, free (and very controversial) needle exchange programs offer everything from cookers to mix drugs to cotton balls used for filtering fillers out of the solution.
4). Stop Using Drugs Intravenously
There is only one sure way to prevent infective endocarditis caused by IV-drug use and that is to stop injecting drugs intravenously. It sounds really simple- and it is really that simple but due to the vicious cycle of addiction, it’s also extremely difficult to quit using drugs- especially once you have crossed the threshold to shooting up.
Why Don’t More People Talk About Endocarditis?
After my battle with infective endocarditis, I wondered why I had never heard of it before it almost killed me. A “seasoned” IV drug user that started injecting when I was 17 and OxyContin was still the opiate of choice and yet I had never even heard of or thought about the possibility of bacteria entering my blood stream. Was it because I was a naïve young kid when I started shooting drugs?
I suspect the reason I had never heard of infective endocarditis before it nearly killed me and took my mitral valve in favor of a St. Jude’s version that requires a daily dose of Warfarin to prevent strokes was simply because nobody wants to talk about things like deadly diseases that kill drug addicts. Least of all the addicts themselves, so instead of talking about it we sit and suffer in silence. Waiting for the day when the addiction finally takes us out of the miserable existence we face in active use.

Leave a Reply